A personalised care approach includes supporting someone to live well with their long term condition.
There is a growing body of evidence that complex population health interventions as a result of patient-centred goal setting, community development and social prescribing have shown highly significant reductions in unplanned admissions to hospital .
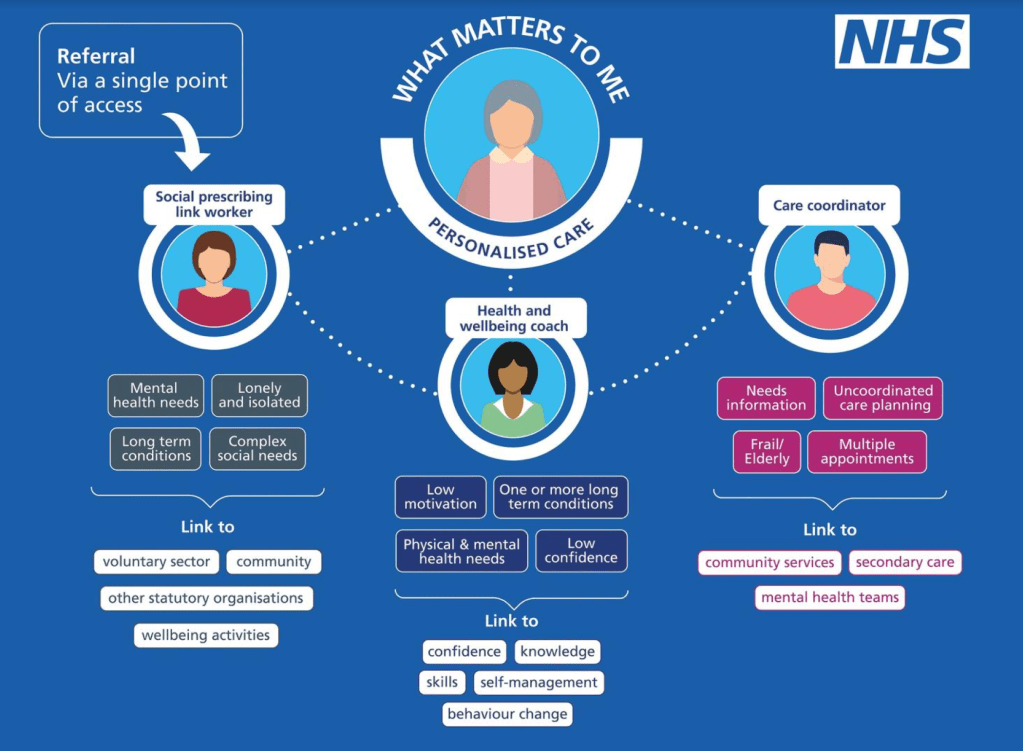
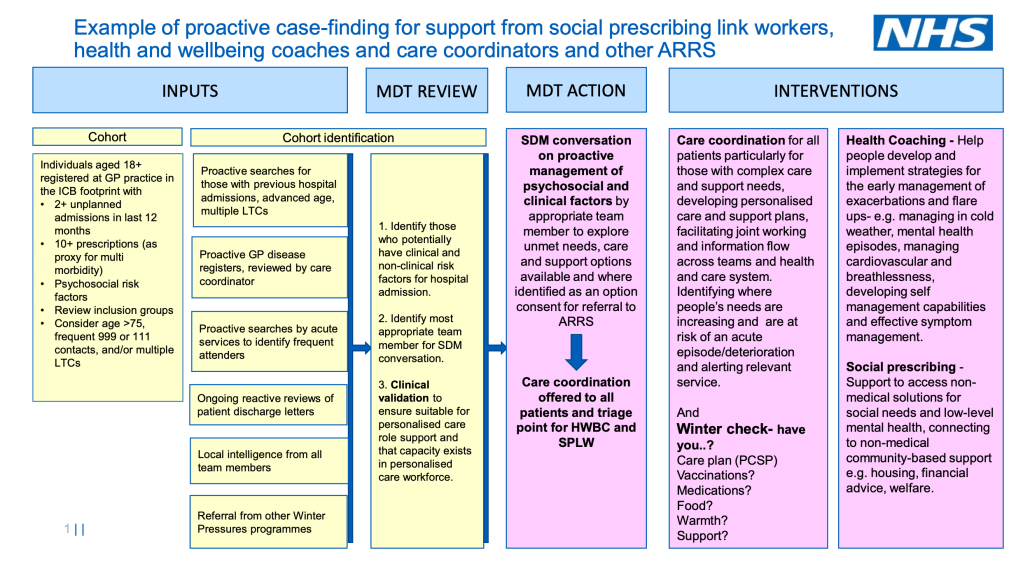
The pathway below sets out practical steps that can be taken by health services to offer proactive personalised care delivered through multidisciplinary teams and maximising the support offered through the three personalised care roles: social prescribing link workers, health and wellbeing coaches and care coordinators with the aim of increasing individual’s knowledge, skills and confidence to better manage their health and wellbeing.
The COVID-19 pandemic has highlighted how how connection to others in our communities can positively impact on our wellbeing. We have seen how health services can use population health to identify and support for people who are identified as more vulnerable to poor physical and mental health.
The personalised care roles have been increasingly uncovering and addressing psychosocial support needs. The roles can also connect people who have a long term physical or mental health condition to peer communities and local services to help people to improve their symptom and condition management so that they can live well.
Integrated care systems are already using population health management data and risk stratification tools including the NHS health inequalities dashboard to develop proactive approaches to supporting patients at highest risk of unplanned admissions or experiencing health inequalities.
Health services, by inviting people who have a long term physical or mental health condition to tell us what issues they are experiencing and what type of support might be most beneficial to them, will be better placed to work with people to more proactively manage their health and wellbeing.
As outlined in Dr. Claire Fuller’s report ‘Next Steps for Integrating Primary Care,’ supporting the growth and development of integrated neighbourhood teams and re-orientating the existing workforce to support our most vulnerable and complex patients to stay at home and access care in the community will, over time, contribute significantly to efforts to impact on the growth in hospital demand.
Health and wellbeing coaches, care coordinators and social prescribing link workers provide an excellent opportunity to address health improvement as well as providing connections to local communities and services and each role has its own unique contribution to make.