
Shared decision making in healthcare is a collaborative process involving a person and their healthcare professional working together to reach a joint decision about their care. The decision is based on choosing tests and treatments based on both evidence and the person’s individual preferences, beliefs and values.
The outcomes of shared decision making are that people feel empowered to make decisions that are right for them at that time.
Enablers for shared decision making include: health professionals skilled in shared decision making, patients being actively involved in decision making about their care and reasonable adjustments for patients, particularly those with lower levels of health literacy. 30minute training for health professionals on shared decision making is freely available from the Personalised Care Institute.

The MAGIC team in Newcastle were supported by The Health Foundation to use CQUIN indicators to embed shared decision making into routine clinical practice using six specific actions. NHS England has included a specific indicator PSS2: Achieving high quality shared decision making conversations in specific specialised pathways to support recovery in recommended specialised acute pathways on page 30 of the CQUIN scheme 2022/23 to support implementation of shared decision making.
Shared decision making enables health professionals to comply with post Montgomery legal requirements to take reasonable care to ensure that the patient is aware of any material risks involved in any recommended treatment and of any reasonable alternative or variant treatments. Shared decision making can support the use of more conservative treatment options.
Since the COVID-10 pandemic two regulatory publications supporting shared decision making have been published: the NICE guideline on SDM and the GMC Guidance on Decision Making and Consent.
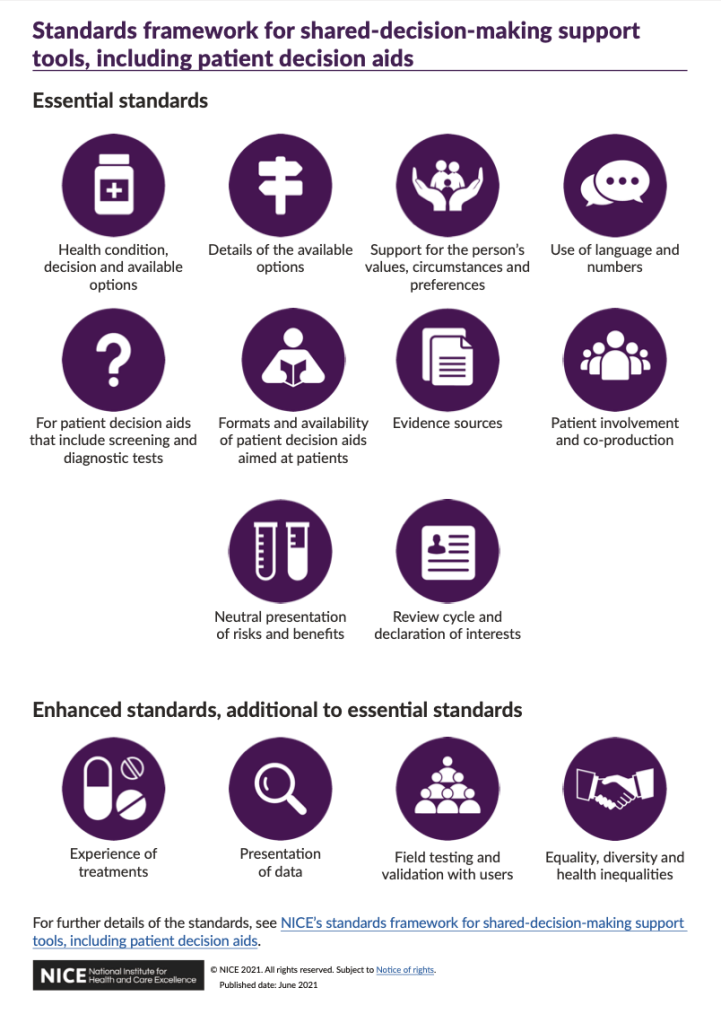
NICE have also published a shared decision making support tool standard framework for those looking to develop shared decision making support tools.
Some decision support tools have already been developed by NICE and NHS England.
Evaluating the impact of shared decision making decision support tools should be looked at through the lenses of the patient experience and clinician experience, while measuring the supportiveness of the system and impact on service utilisation over time.
Further reading on guidance and resources on shared decision making.